NEC in the NICU: Understanding Stages, Symptoms, and Treatment
Necrotizing Enterocolitis (NEC) in Newborns: Causes, Symptoms, Diagnosis & Management
Necrotizing enterocolitis (NEC) is one of the most serious gastrointestinal emergencies in newborns, especially in premature infants. It involves inflammation and death (necrosis) of intestinal tissue. Without timely treatment, it can lead to life-threatening complications. Early recognition and prompt management are essential to improve outcomes
What Is Necrotizing Enterocolitis?NEC is an inflammatory condition in which segments of the bowel wall become injured, inflamed, and may eventually die. The disease primarily affects premature babies, especially those with low birth weight, though it can also occur in term infants under certain risk factors.
Who Is at Risk?
Although NEC can affect any newborn, the risk is significantly higher in the following situations:
1. Prematurity
-
Most cases occur in infants born before 32 weeks gestation.
-
Premature infants have immature immunity, weak gut barriers, and poor blood flow regulation.
2. Formula Feeding
-
Formula-fed infants are at greater risk compared to breastfed infants.
-
Breast milk provides antibodies and growth factors that protect and mature the infant’s gut.
3. Intestinal Ischemia
-
Reduced blood flow to the bowel (due to shock, congenital heart disease, or sepsis) increases the risk.
4. Abnormal Bacterial Colonization
-
Premature infants may acquire harmful bacteria early in life, especially in the NICU setting.
5. Other Contributing Factors
-
Rapid feeding advancement
-
Prolonged antibiotic use
-
Exchange transfusion
-
Indomethacin therapy
Signs and Symptoms of NEC we have Gastrointestinal Symptoms and Systemic Symptoms
How Is NEC Diagnosed?
1. Physical Examination
2. Imaging
3. Laboratory Tests
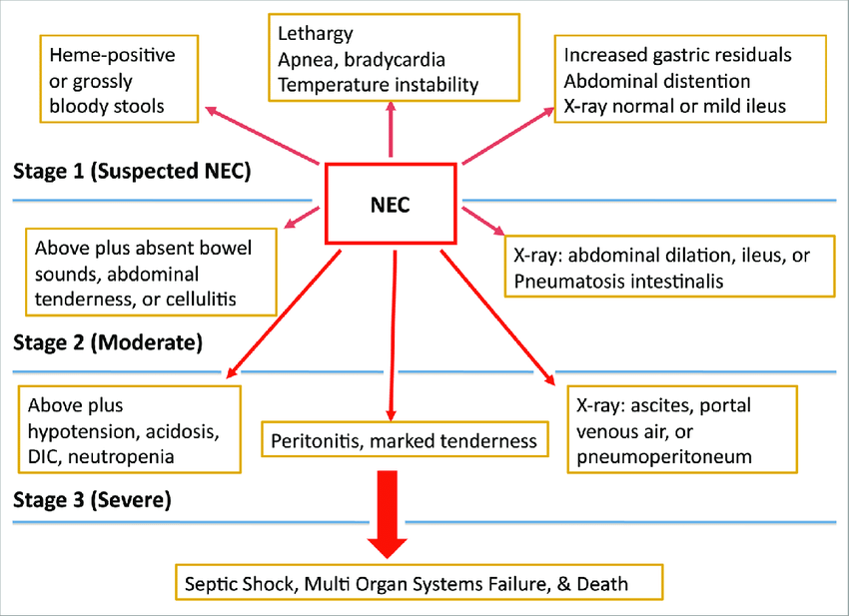
NEC Staging (Modified Bell’s Stages)
Stage IA–IB: Suspected NEC (Mild)
These early stages involve mild symptoms such as slight abdominal distension and the presence of occult (hidden) or visible blood in the stool. At this point, NEC is suspected based on clinical signs but not confirmed by imaging.
Stage IIA–IIB: Proven NEC (Moderate)
In these stages, NEC is confirmed. The infant shows radiologic signs such as pneumatosis intestinalis (air within the bowel wall). Other features may include portal venous gas and metabolic acidosis. Symptoms are more pronounced, and the infant shows definite intestinal involvement.
Stage IIIA–IIIB: Advanced NEC (Severe)
These are the most severe stages. Infants may have bowel perforation, leading to free air in the abdomen. Peritonitis, severe systemic illness, worsening acidosis, and signs of shock may be present. Stage IIIB specifically involves perforation, while Stage IIIA is severe NEC without perforation.
1. Medical Management (Early or Moderate NEC)
2. Surgical Management (Severe NEC)
Possible Complications
Prevention
1. Exclusive Breast Milk Feeding
2. Probiotics
3. Slow Feeding Advancement
4. Strict Infection Control
5. Kangaroo Mother Care
Necrotizing enterocolitis (NEC) is one of the most serious gastrointestinal emergencies in newborns, especially in premature infants. It involves inflammation and death (necrosis) of intestinal tissue. Without timely treatment, it can lead to life-threatening complications. Early recognition and prompt management are essential to improve outcomes.
NEC is an inflammatory condition in which segments of the bowel wall become injured, inflamed, and may eventually die. The disease primarily affects premature babies, especially those with low birth weight, though it can also occur in term infants under certain risk factors.
Although NEC can affect any newborn, the risk is significantly higher in the following situations:
-
Most cases occur in infants born before 32 weeks gestation.
-
Premature infants have immature immunity, weak gut barriers, and poor blood flow regulation.
-
Formula-fed infants are at greater risk compared to breastfed infants.
-
Breast milk provides antibodies and growth factors that protect and mature the infant’s gut.
-
Reduced blood flow to the bowel (due to shock, congenital heart disease, or sepsis) increases the risk.
-
Premature infants may acquire harmful bacteria early in life, especially in the NICU setting.
-
Rapid feeding advancement
-
Prolonged antibiotic use
-
Exchange transfusion
-
Indomethacin therapy
NEC typically appears within the first 2–6 weeks of life. Symptoms may start subtly but can worsen quickly.
-
Abdominal distension (bloated or swollen abdomen)
-
Feeding intolerance or vomiting
-
Blood in stool
-
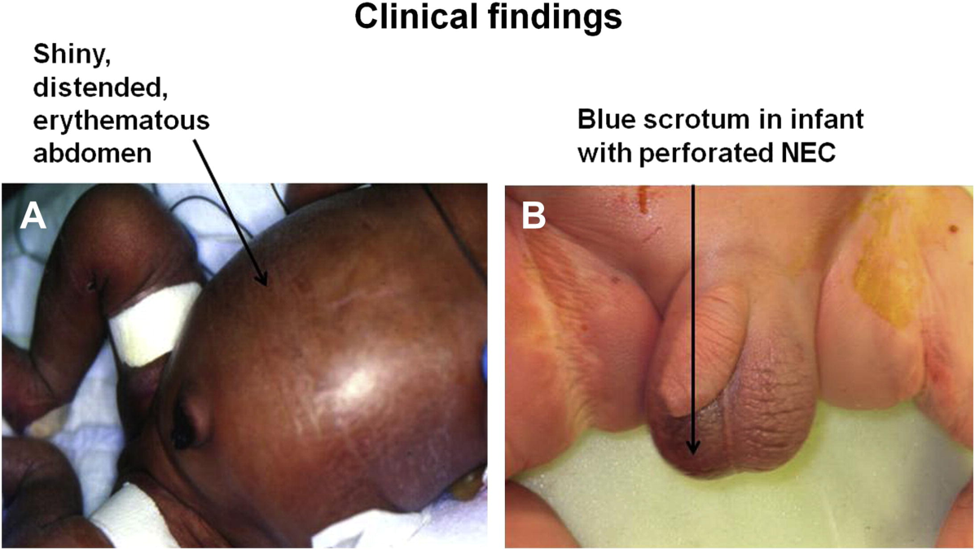
Abdominal discoloration (bluish or reddish patches)
-
Lethargy
-
Temperature instability
-
Apnea (pauses in breathing)
-
Bradycardia (slow heart rate)
-
Poor perfusion or signs of shock
Immediate medical evaluation is critical when these symptoms appear.
Diagnosis combines clinical assessment with imaging and laboratory tests.
-
Distended, tender abdomen
-
Visible abdominal veins or skin discoloration
Abdominal X-ray is the key diagnostic tool. It may reveal:
-
Pneumatosis intestinalis (air in the bowel wall) — hallmark sign
-
Dilated bowel loops
-
Portal venous gas
-
Pneumoperitoneum (free air) if perforation occurs
-
CBC: leukocytosis or leukopenia
-
Thrombocytopenia (low platelets)
-
Elevated CRP
-
Metabolic acidosis
-
Positive blood cultures (if sepsis is present)
Management strategies depend on the stage and severity of the illness.
-
Stop all enteral feeds (NPO)
-
Nasogastric tube for gastric decompression
-
Broad-spectrum IV antibiotics
-
IV fluids and total parenteral nutrition (TPN)
-
Respiratory support if needed
-
Frequent abdominal assessments and serial X-rays
Most infants respond to medical treatment within 7–14 days.
Surgery is required when:
-
Bowel perforation is present
-
Worsening metabolic acidosis
-
Peritonitis develops
-
Medical therapy fails
Surgical options include:
-
Peritoneal drain placement
-
Laparotomy with removal of dead bowel
-
Creation of an ostomy if necessary
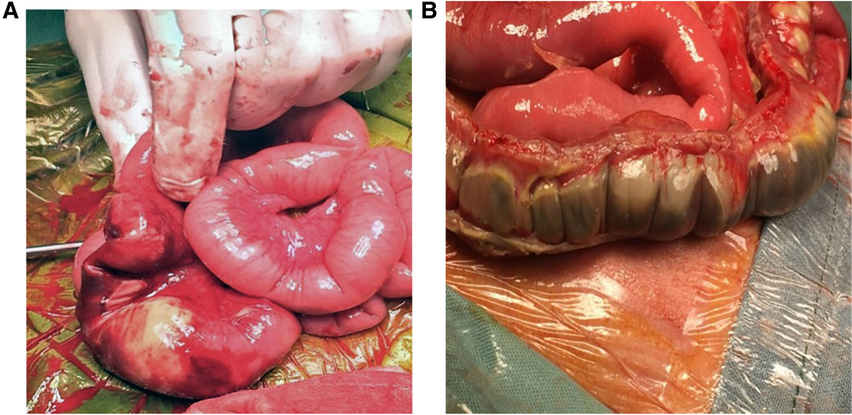
Extensive bowel removal may result in short bowel syndrome.
-
Intestinal strictures
-
Short bowel syndrome
-
Sepsis and shock
-
Failure to thrive
-
Neurodevelopmental delays
-
Mortality
NEC remains a major cause of illness and death in neonatal intensive care units worldwide.
Although NEC cannot always be prevented, several strategies significantly reduce risk:
-
Provides the strongest protection
-
Donor breast milk is preferred when mother’s milk is unavailable
-
Some NICUs use probiotics to promote healthy gut bacteria (practice varies)
-
Gradual increase in feeding volumes reduces stress on the gut
-
Proper hand hygiene
-
Minimizing invasive procedures
-
Skin-to-skin care supports immunity and gut function
Understanding necrotizing enterocolitis (NEC) is essential for both academic learning and clinical practice. Because NEC progresses rapidly and can lead to severe complications, early recognition of symptoms and accurate staging play a critical role in improving outcomes for newborns. This article provides a clear and practical guide to the causes, risk factors, clinical features, diagnosis, and management of NEC—knowledge that is vital for students, healthcare providers, and anyone involved in neonatal care. By combining educational depth with clinically useful information, the goal is to support better decision-making and promote timely, effective intervention for infants at risk.